Parents or caregivers often struggle to differentiate between self-harm and suicide behaviors (includes suicidal thoughts, plans, or history of suicide attempts.
Self-Harm: A Misunderstood Cry for Help
In Self-harm, also known as Non-Suicidal Self-Injury (NSSI), the attempt is not to take one’s life. It might seem counterintuitive, but for some people, self-harm becomes a coping mechanism. The pain (whatever the source could be) becomes a way to deal with overwhelming emotions such as intense sadness, anger, or anxiety. It can also be a way to feel something when feeling numb or disconnected.
Suicide Behavior: A Different Kind of Pain
Suicide Behavior includes three categories: suicidal thoughts, plans and history of suicide attempts. Unlike self-harm, suicide attempts stem from a place of deep despair and a desire to escape unbearable suffering.
The Bottom Line: Intent Matters
The key difference between self-harm and suicide attempts lies in intent. Self-harm is a cry for help, a way to manage overwhelming emotions, while suicide attempts are fueled by a desire to end those emotions permanently.
Recently, we presented our work at the International Conference on Applying Psychology for Suicide Prevention, Vadodara.
This research examined self-harm as a predictor of suicide behaviour. While self-harm itself doesn’t involve suicidal intent, it highlights vulnerability and warrants attention for suicide prevention and management.
Key Findings:
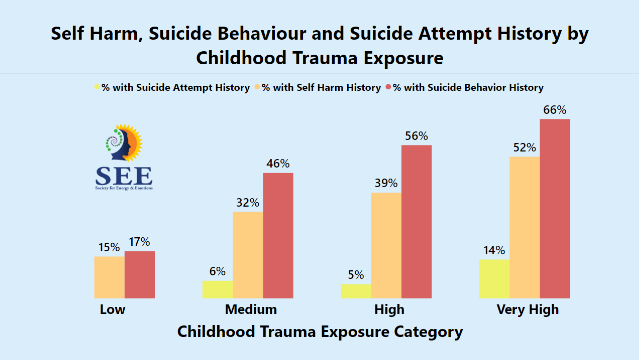
- With an increase in exposure to childhood trauma, the risk for self-harm increases. The visual shows that individuals exposed to very high childhood trauma have a higher risk for both self-harm and suicide behaviour compared to those who are exposed to low levels of childhood trauma.
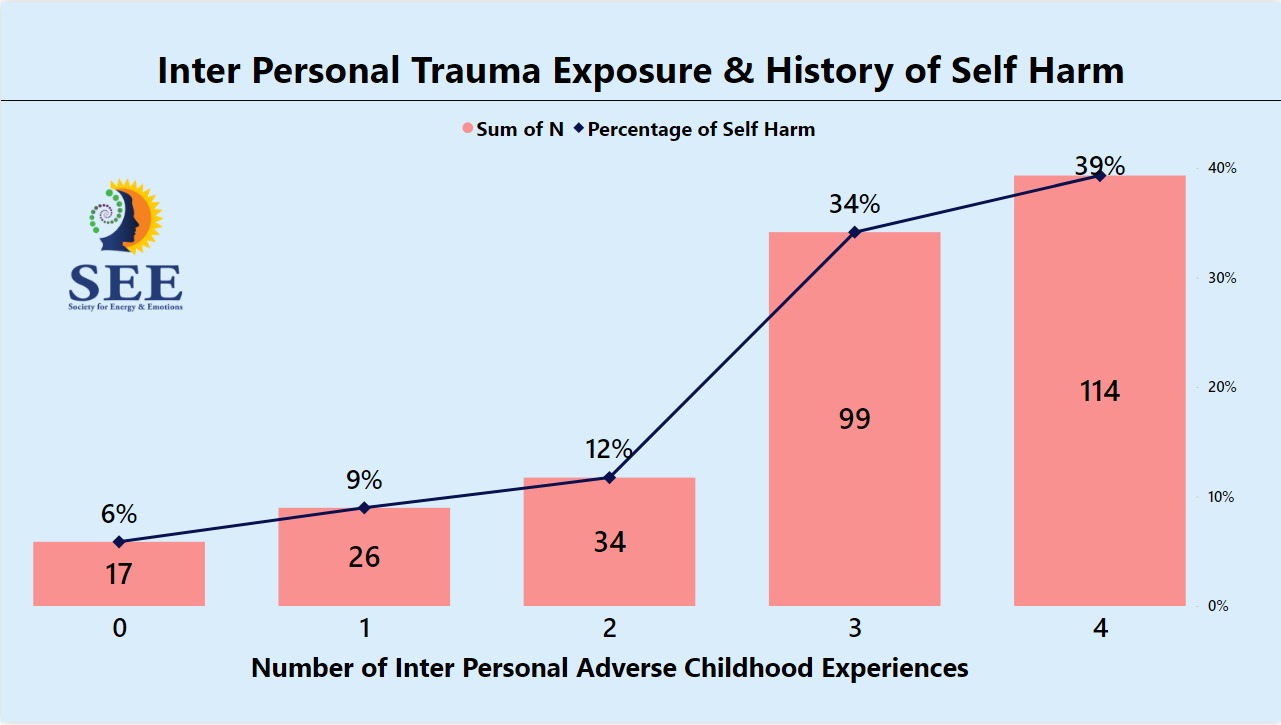
- Interpersonal childhood trauma components (or ACEs: Adverse Childhood Experiences) play a significant role in increasing the risk for self-harm. These components include (a) Emotional abuse, (b) Physical Abuse, © Sexual Abuse, (d) Emotional Neglect, (e) Domestic violence (or intimate partner violence), and (f) Parents fighting (verbal).
- The logistic regression model highlighted that individuals with at least 3 of these 6 interpersonal trauma experiences are about three times more likely to experience self-harm.
- The risk increases with an increase in exposure to interpersonal trauma components. Individuals who are physically violent to others are also 3 times more likely to experience self-harm. The issue is more prevalent in younger individuals (compared to older).
How do we assess and address such issues?
The following are unique aspects of how we assess and address the root causes of issues such as self-harm or suicide behaviour.
- Granular Analysis: We assess all the childhood experiences involving trauma, and hence we also understand the extent of exposure to interpersonal trauma components highlighted earlier. We also noted additional risk factors such as violent behavior tendencies.
- Evidence-Based Approach: The study utilizes established methods like the Adverse Childhood Experiences (ACE) questionnaire and the 80/20 rule-based index trauma assessment to ensure strong, verifiable results.
- Intervention Techniques: The research continues beyond diagnosis. It highlights therapeutic approaches like Inner Child Integration Therapy and Reconsolidation of Traumatic Memories (RTM) that target emotional neglect and its lasting effects. These interventions are part of the Integrated Regression Therapy & Life Coaching Certification training.
What it Means for You:
This research offers a glimmer of hope for those who have the risk of self-harm or suicide behaviour. Acknowledging the potent roles of risk factors, therapists can tailor treatment plans to address the root cause of the problem. Techniques like Inner Child Integration and RTM empower individuals to heal past hurts and build resilience.
Watch this video to here about this research:





Leave A Comment